Screening of HPV vaccinated women
Dr. Eduardo Franco contemplated the difficult decisions facing health care providers in the foreseeable future in maintaining current standards of thoughts in screening due to decreasing background exposure to HPV which will result from the implementation of national HPV vaccination programs.
Primary prevention of cervical and other HPV-associated cancers by vaccination will reduce not only the prevalence of precursor lesions but also the prevalence of the high-risk (hr) HPV types that can be detected by screening aimed for the prevention cervical cancer.
This prevalence reduction will result in the decrease of the positive predictive value of even the most accurate screening tests with up to 99% sensitivity and specificity for the identification of hrHPV DNA.
After reaching a critical threshold level of 0.2% in the prevalence of precursor cervical lesions, we can predict a rapidly increase in the rates of false positive findings irrespectively of the accuracy of any of the tests used(table 1).
Eventually the impact of vaccination, most importantly due to the decreasing background exposure/prevalence of precursor lesions, will affect even a number of the present benefits of HPV DNA testing:
- safety of increasing screening interval
- potential of self-collected samples in the unscreened sub-populations
- detection of cervical adenocarcinoma precursors
- simplicity of algorithms
In the foreseeable future, screening for cervical cancer may cease to fulfil the revised Wilson and Jungner criteria [1] for an applicable screening test. Eventually, the screening for cervical cancer in the vaccinated population probably will need to be abandoned due to the fact that the damage of over-diagnosis and over-treatment will outweigh the benefits of screening.
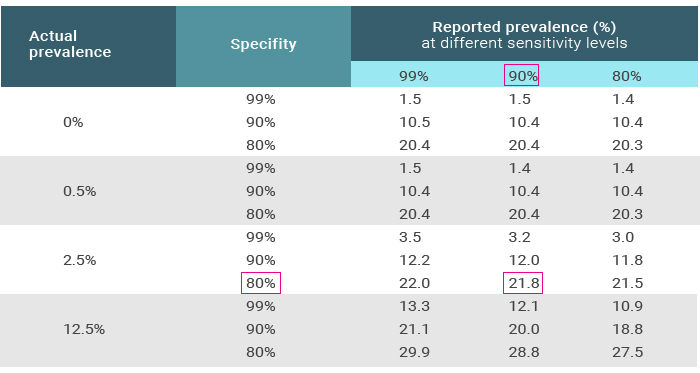
Table 1. The impact of reducing background prevalence on the true identification of HPV types.
Text-legend: The circle indicates the reported prevalence of a given HPV type in a screening environment (21.8%) using a test with 90% sensitivity and 80% specificity when the actual prevalence of the virus in the population is 2.5%. Most screen positive results will indeed be false-positive leading to over-diagnosis and over-treatment. Notice that unless very careful audits of the screening programs are conducted, most overdiagnostic procedures including treatments passed largely unnoticed to the system. Adapted from [2].
References
1. Andermann A, Blancquaert I, Beauchamp S, Déry V. Revisiting Wilson and Jungner in the genomic age: a review of screening criteria over the past 40 years. Bull WHO, 2008. 86:p.241-320.
2. Franco EL. The sexually transmitted disease model for cervical cancer. Incoherent epidemiologic findings and the role of misclassification of human papillomavirus infection. Epidemiology. 1991; 2: 98-106.
