Parents hesitancy about HPV vaccination
Despite recommendations for routine HPV vaccination from the World Health Organization and many national governments, many parents remain hesitant about vaccinating their children against human papillomavirus (HPV). For instance, in the United States, only 43% of adolescents had completed the recommended vaccination series in 2016, which is substantially lower than other adolescent vaccines.1 Furthermore, despite initially high uptake, some countries have witnessed dramatic declines in HPV vaccination rates, including, for example, Colombia and Ireland (Figure 1). Although other countries have maintained success with HPV vaccination (e.g. Australia), clearly HPV vaccine hesitancy remains an obstacle to achieving desired reductions in HPV-related cancer rates in some locales (Figure 1).
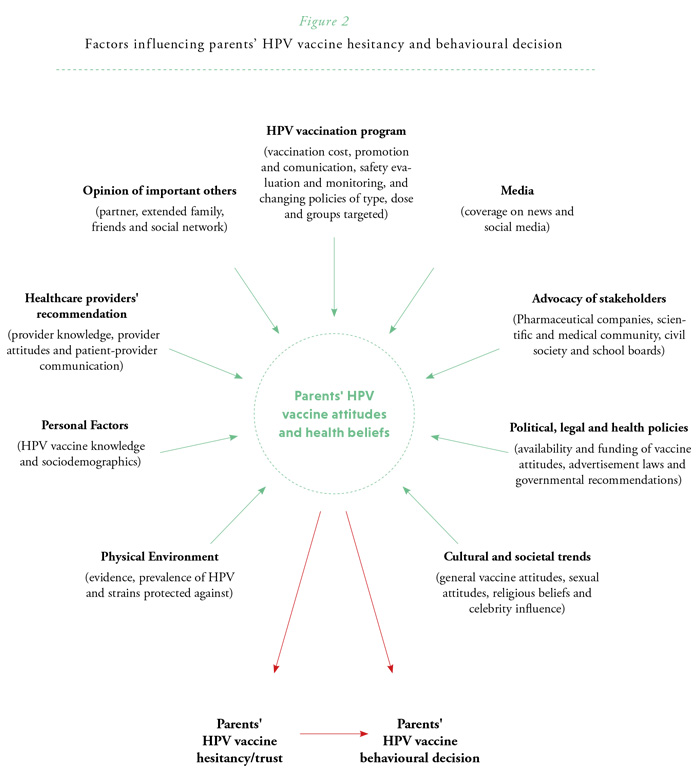
Understanding parents’ HPV vaccine hesitancy Parents’ attitudes towards HPV vaccination decision-making for their children are complex, multilayered, and influenced by a number of factors (Figure 2). Over the last decade, the evidence has indicated some common themes such as the importance of parents’ believing in the many benefits and few barriers of HPV vaccination.2 Unsurprisingly, parents are less likely to vaccinate their children if they believe that the HPV vaccine can cause harm, or that the vaccine is not accessible or affordable. Furthermore, parents are more likely to vaccinate their children if they perceive HPV infection and associated disease to be severe and that their child is at risk of contracting HPV. In addition, positive attitudes towards vaccines in general (e.g. low vaccine conspiracy beliefs or high trust in a countries’ vaccine recommendation and programs) are related to HPV vaccination.
While the importance of these attitudes for vaccination is clear, the degree to which each of these factors contributes to vaccination behaviours remains largely unclear. Furthermore, parents can hold multiple and conflicting attitudes at one time. For example, parents may believe their child is at risk for an HPV-associated cancer, but also be concerned about vaccine side effects. HPV vaccine attitudes also are not held in a vacuum but are influenced by social and societal factors.3-5 Notably, a strong healthcare provider’s recommendation significantly improves parental vaccine acceptance.2 Other relationships in parents' orbit—including their partner, extended family, friends, and online social network—can influence parents’ attitudes both for and against vaccination. In addition, broader political and cultural trends—such as general attitudes towards vaccination, sexual attitudes, and changing policies regarding HPV vaccine type, dose, and groups targeted for vaccination—can shape parents’ attitudes.

Note. Data refers to female HPV vaccine uptake rates. The uptake rates from these three countries represent a different number of doses of the HPV vaccine. Rates are intended to demonstrate a trend rather than a cross-country comparison.
Data was compiled from the following sources:
1) Health Protection Surveillance Centre. 2018. “HPV vaccine uptake in Ireland: 2016/2017”. Dublin Ireland.
Accessible at: http://www. hpsc.ie/a-z/vaccinepreventable/vaccination/immunisationuptakestatistics/hpvimmunisationuptakestatistics/;
2) Vorsters, A., et al. Nubia Muñoz, Raul Murillo, Pierre Van Damme, Emilie Karafillakis, Silvia de SanJosé, Laia Bruni, Heidi Larson. 2017. “Colombia: Decreasing HPV vaccination coverage: mapping roles of different stakeholders and societal-historical factors”. Poster presentation at HPV symposium: Building Trust, Managing Risk: Vaccine Confidence and Human Papillomavirus Vaccination, 7-8 June 2017.
Accessible at: http://www. vaccineconfidence.org/hpv-symposium/;
and 3) Australian Government Department of Health. 2018. National HPV Vaccination Program Register.
Accessible at: http://www.hpvregister.org.au/research/coverage-data.
The importance of theoretical models to influence and evaluate parents’ decision-making Given the multiple variables that impact health decisions like this, it is important to design theoretically informed and methodologically rigorous interventions to assess what strategies might be most effective in improving vaccination rates. Behavioural science theories such as the Health Belief Model, the Theory of Planned Behaviour and the Precaution Adoption Process Model provide strong theoretical foundations for identifying relevant variables including attitudes, perceptions of severity and susceptibility, social normative influences, and facilitators and barriers to behaviour, which can then be used to design tailored interventions for different parent populations. We must now focus more attention on evaluation of theoretically-informed and rigorous interventions strategies in order to achieve change in vaccine hesitant parents.
Summary
The reasons for parents’ HPV vaccine hesitancy are complex. To ensure the success of HPV vaccination programs, we must pursue research that evaluates psychosocial factors alongside studies of safety and efficacy. Further, behavioural scientists must focus on identifying intervening variables through the use of theoretically informed and methodologically rigorous intervention studies that incorporate a wider perspective of potential influences. Only in this way can we ensure that HPV vaccination rates increase (and remain high) so that HPV cancer prevention goals can be met.

References
1. Walker TY, Elam-Evans LD, Singleton JA et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 Years — United States, 2016. MMWR Morb Mortal Wkly Rep 2017; 66:874–882.
2. Holman DM, Benard V, Roland KB et al. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr 2014;168(1):76-82.
3. Head KJ, Biederman E, Sturm LA et al. A retrospective and prospective look at strategies to increase adolescent HPV vaccine uptake in the United States. Hum Vaccin Immunother 2018;14(7):1626-1635.
4. Dube E, Laberge C, Guay M et al. Vaccine hesitancy: An overview. Human Vaccines & Immunotherapeutics 2013;9(8):1763–1773.
5. Shapiro GK, Guichon J, Prue G et al. A Multiple Streams analysis of the decisions to fund gender-neutral HPV vaccination in Canada. Prev Med 2017;100:123-131.



