Elimination of cervical cancer from developing countries
Dr. Franceschi focused on the estimated world-wide number of cancers attributable to infections in 2012 (table 1), the trends in HPV-associated cancer rates, and monitoring progress of cervical cancer prevention by screening and vaccination [1, 2]. Country-wide, the fraction of cancer attributable to infections is highly correlated with the country-specific income (figure 1). The annual number of new HPV-associated cancer cases is 650.000, the vast majority being cervical cancer. Cancers in males (mostly oropharyngeal, anal and penile) comprise approximately 10% of all HPV-induced cancers. In 2012 cervical cancer continued to be the most frequent cause of premature cancer death in low and middle income countries (LMICs). This is not so much due to differences in the prevalence of cervical HPV infection in 15-59 year-old women, but in the different availability of organized screening programs. Such programs are in place in some, but not all high-income countries, which indicates, that economical improvements are not sufficient to tackle HPV infection but screening and HPV vaccination are needed. While screening can be effective, it is much more logistically demanding than vaccination. Screening can prevent invasive cancer in individual women rapidly but it typically requires ≥10-20 years to achieve high coverage and a high quality of the entire screening, diagnostic and treatment process.
Especially in the context of the Low and Middle Income Countries (LMICs), the open questions today for HPV-based screening programs are: 1. Age to start and stop screening activities considering the risk and the costs of over-diagnosis and over-treatment of lesions that would spontaneously regress in the absence of any treatment, a frequent event in young women, 2. Triage strategies for HPV-positive women to decide on the treatment necessity, and 3. Adequate screening programs of vaccinated women.
As for HPV vaccination, policy-makers in many countries are understandably afraid of investments that will take decades to produce fully accountable results. However, HPV vaccination is highly feasible compared to that of other cancer prevention strategies, especially in the LMICs and many countries (close to 60 in 2015) have already included HPV vaccination in their routine vaccination schemes. Moreover, the Global Alliance for Vaccination and Immunization (GAVI) has also added HPV vaccination to their portfolio and several countries have imitated vaccination. Unfortunately, cancer registries in many of the LMICs may not be up to the task of monitoring post vaccination reductions in HPV-related cancers.
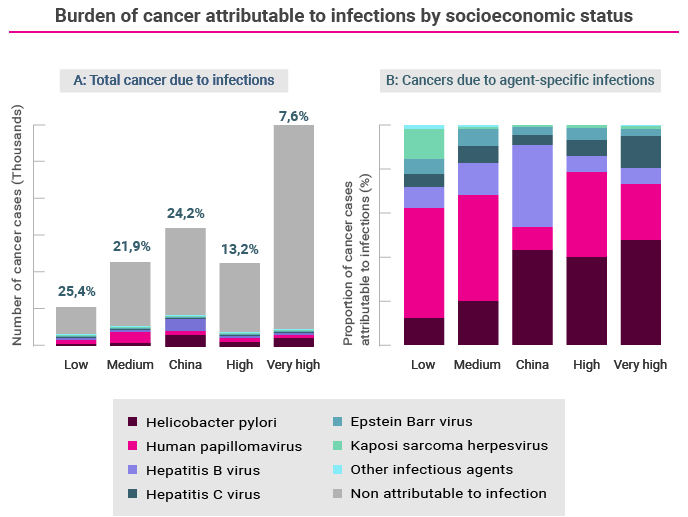
Figure 1. Panel A: Correlation of fraction of cancers attributable to infections by region/country-specific income (low to very high). Panel B: Infectious agent-specific infections as a % of all infection induced cancers by income. Colours indicate the relative proportions of different infectious/non-infectious causes of cancer. Reproduced with permission [2].

Table 1: Number of cases of cancer per year attributable to infectious agents by region.
References
1. Schiffman M, Doorbar J, Wentzensen N, et al. Carcinogenic human papillomavirus infection. Nat Rev Dis Primers, 2016. 2:p.16086.
2. Plummer M, de Materl C, Vignant J, et al. Global burden of cancers attributable to cancers in 2012: a synthetic analysis. Lancet Global Health 2016. 4:e609-629.
