Reproductive impact of local CIN treatment
Why is the impact of conisation on reproduction important?
The introduction of systematic call and recall screening programmes has resulted in a substantial decrease in the incidence and mortality from cervical cancer as pre-invasive precursors (cervical intra-epithelial neoplasia; CIN) can be detected by the screening programme and treated. In England alone, 3.6 million women aged 25 to 64 attended for screening in 2013-14 and over 22000 treatment procedures were carried out.
The mean age of women undergoing CIN local treatment is similar to the age of women having their first child. The impact that conisation may have on their future ability to carry a healthy and successful pregnancy is important to the majority of the treated population. Although, previously, complications from treatment were thought to be relatively mild and uncommon, an increasing body of retrospective observational studies and meta-analyses published in the last decade suggested that treatment, particularly excision, adversely affects future reproduction and the risk of prematurity.
Outpatient large loop excision of the transformation zone (LLETZ) is the preferred treatment of choice in most settings, although clinical practices vary across Europe and beyond. In some European countries, knife excision (cold knife conisation [CKC]) is still regularly performed; in others, laser ablation or laser excision is common practice.
What is the impact of conisation on fertility?
Although the evidence is limited, a meta-analysis of 15 studies concluded that there appears to be no impact of local cervical treatment on the ability to conceive.1 The overall pregnancy rate was higher for treated versus untreated women (4 studies; 43% vs 38%; relative risk [RR] 1.29, 95% CI 1.02–1.64), while the pregnancy rate in women with an intention to conceive was similar (2 studies; 87.9% vs 94.6%; RR 0.93, 95% CI 0.80– 1.08). The rate of women requiring more than 12 months to conceive were higher for treated versus untreated women, although the difference was not significant (3 studies; 14.7% vs 9.2%; RR 1.45, 95% CI 0.89–2.37); this may however be explained by clinicians’ recommendation to delay conception until after the early post-operative period. The impact of repeat and large cones on fertility remains unclear as limited evidence does not permit stratification of risk.
What is the impact of local treatment on early pregnancy up to 24 weeks of gestation?
A recent meta-analysis reported that local treatment significantly increased the risk of 2nd trimester miscarriage compared with untreated controls (8 studies; 1.6% vs 0.4%; RR 2.6, 95% CI 1.45–4.67). The rates of overall and 1st trimester miscarriages were similar, although treated women had increased rates of ectopic pregnancy and termination of pregnancy.1

What is the impact of local treatment on obstetric outcomes after 24 weeks of gestation?
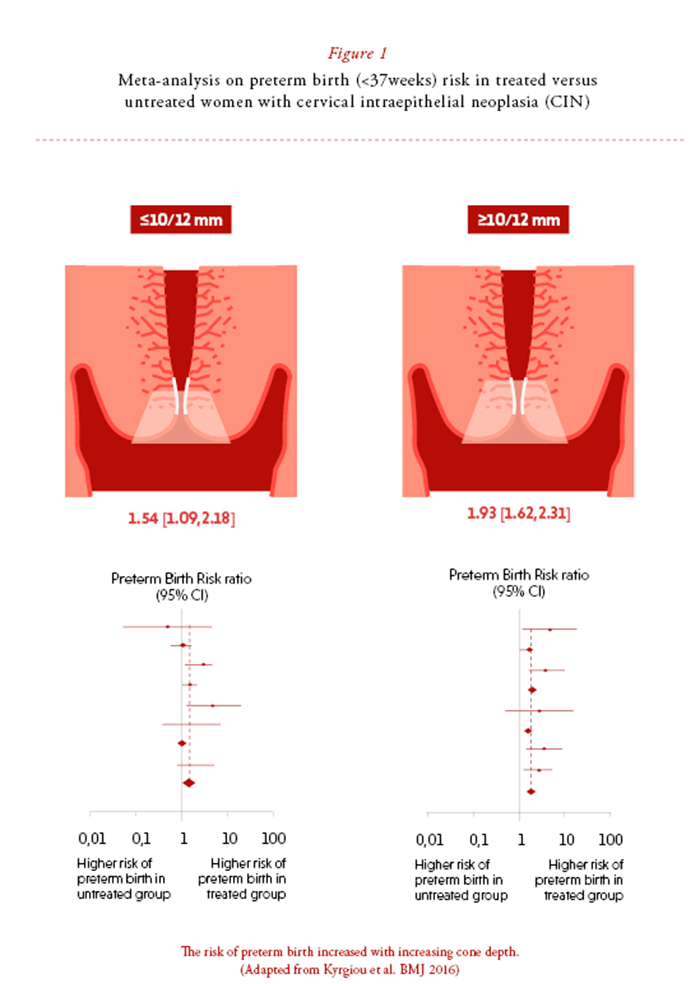
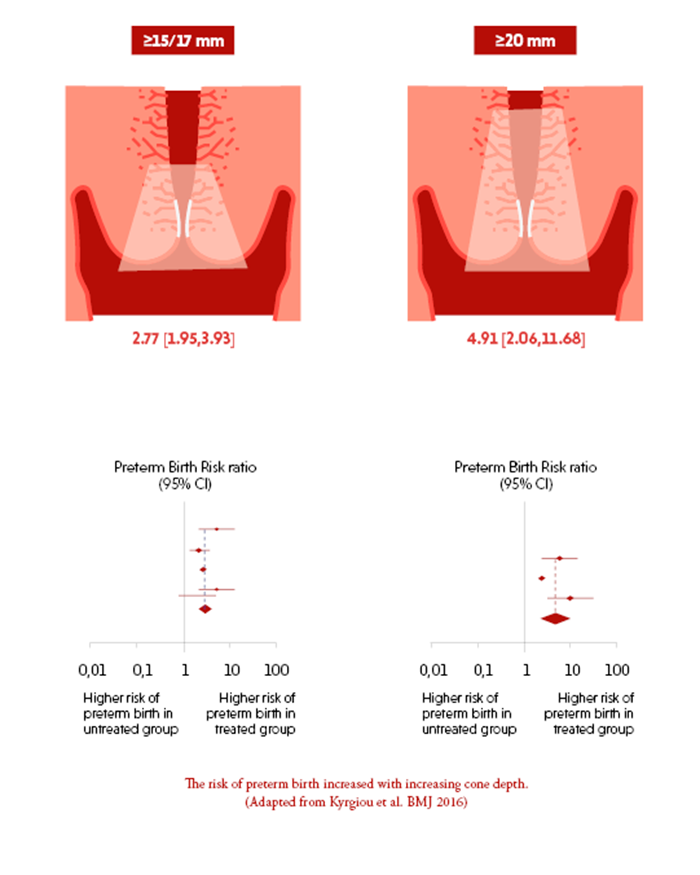
Local treatment has been associated with increased adverse outcomes in subsequent pregnancies. A recent update in 2016 of the original meta-analysis published in 20062 included 71 studies (6 338 982 participants: 65 082 treated/6 292 563 untreated).3 Local treatment was associated with an increased risk of overall ( < 37 weeks; 10.7% vs 5.4%; RR 1.78, 95% CI 1.60-1.98), severe ( < 32-34 weeks; 3.5% vs 1.4%; 2.40, 1.92-2.99), and extreme ( < 28-30 weeks; 1.0% vs 0.3%; 2.54, 1.77-3.63) preterm birth. The frequency and severity of the observed adverse events was higher for the more radical techniques, for excision than for ablation and with increasing cone depth. The relative risk of preterm birth ( < 37 weeks) was 2.70 (2.14-3.40) for CKC, 2.11 (1.26-3.54) for laser conisation, 2.02 (1.60-2.55) for excision not otherwise specified, 1.56 (1.36-1.79) for LLETZ, and 1.46 (1.27-1.66) for ablation not otherwise specified (table 1). Compared with no treatment, the preterm birth rate was higher for women after more than one local treatment (13.2% vs 4.1%; 3.78, 2.65-5.39) and with increasing cone depth (≤10-12 mm; 7.1% vs 3.4%; 1.54, 1.09-2.18; ≥10-12 mm: 9.8% vs 3.4%, 1.93, 1.62-2.31; ≥15-17 mm: 10.1% vs 3.4%; 2.77, 1.95-3.93; ≥20 mm: 10.2% vs 3.4%; 4.91, 2.06-11.68) (figure 1). Spontaneous preterm birth, premature rupture of the membranes, chorioamnionitis, low birth weight, admission to neonatal intensive care, and perinatal mortality were increased after treatment. This analysis also confirmed that women with untreated CIN belong to a high-risk population with an increased baseline risk of prematurity when compared to the general population (5.9% v 5.6%; 1.24, 1.14 to 1.35).
What causes reproductive morbidity in this population?
The mechanism that leads to increased risk of 2nd trimester loss and preterm birth associated with CIN and its treatment is not yet clarified.4 Ascending infection from the vagina into the fetoplacental unit and associated inflammation are presumed to be causative in preterm labour. While acquired mechanical weakness of the cervix secondary to surgery might seem a logical assumption, more subtle mechanisms may be involved that may include histological changes in the healed cervix affecting the tensile strength. Removing part of the cervix or simply being infected with human papillomavirus (HPV) may also impair the host’s defence mechanisms, change the chemical microenvironment and prevent a pregnancy being maintained to full term. Conversely, it may be that women at risk have intrinsic compromised defences that promote the persistence of oncogenic HPV infections and the development of ascending infections during pregnancy.
What can we conclude and what is needed in the future?
Women with CIN are at higher risk of prematurity even without treatment. Local treatment increases further the risk of mid-trimester loss and preterm birth. The risk is higher for excisional rather than ablative techniques and increases with increasing cone depth. This evidence should be available for effective patient counselling at colposcopy and antenatal clinics. In the event of pregnancy, particularly women with large or repeat conisations should be considered high risk for preterm birth. Further research is required to establish the value of antenatal interventions.
The impact of the treatment method and radicality on the chances of future pre-invasive or invasive recurrence should be carefully balanced against the reproductive morbidity. Treatment should always be tailored to treat disease effectively, and at the same time minimise reproductive sequelae. Clearance of the disease at the margins has been associated with substantial reduction in the risk of disease recurrence.5 Future research should aim to generate a clinically useful ranking of alternative options of treatment according to their efficacy, morbidity and cost-effectiveness.
Future research should also explore the mechanisms that lead to adverse reproductive outcomes in this population. A better understanding of pathogenic factors may enable identification of women at risk and the development of cause-directed treatments that could prevent adverse sequelae in the future.

References
1. Kyrgiou M, Mitra A, Arbyn M et al. Fertility and early pregnancy outcomes after treatment for cervical intra-epithelial neoplasia: a systematic review and meta-analysis of the literature. BMJ 2014; 28:g6192
2. Kyrgiou M, Koliopoulos G, Martin-Hirsch P et al. Obstetric outcomes after conservative treatment for intraepithelial or early invasive cervical lesions: Systematic review and meta-analysis. Lancet 2006; 367:489-498.
3. Kyrgiou M, Athanasiou A, Paraskevaidi M et al. Adverse obstetric outcomes after local treatment for cervical preinvasive and early invasive disease according to cone depth: systematic review and meta-analysis. BMJ 2016; 28:i3633
4. Kyrgiou M, Martin-Hirsch P, Paraskevaidis E, Bennett P. Reproductive Outcomes after Local Treatment for Preinvasive Cervical Disease (Scientific Impact Paper No. 21) https://www.rcog.org.uk/en/guidelines-research-services/ guidelines/sip21/ (Accessed 12 December 2018).
5. Arbyn M, Redman CWE, Verdoodt F, Kyrgiou M et al. Incomplete excision of cervical precancer as a predictor of treatment failure: a systematic review and meta-analysis. Lancet Oncol 2017; 18:1665-1679.
